This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome to The Curbsiders. I'm Dr Matthew Frank Watto, here with America's primary care physician, Dr Paul Nelson Williams. Paul, are you excited to do a video with dental care tips for the internist?
Paul N. Williams, MD: It's a topic that has filled me with a bit of anxiety in the past, but I feel much better prepared after speaking with our phenomenal guest who gave us a lot of great practical tips to help me out with some common concerns.
Watto: Dr Lisa Simon was our guest, a former dentist, now an internist. What did she tell us about dry mouth? Any tips?
Williams: Tons of tips. It's a common concern and many things can cause it, such as autoimmune diseases, including Sjögren's. When you're doing your exam, those patients can have fairly striking pathology. The tongue might be reflective because of the loss of papilla. It's kind of shiny and bright, and uniform in appearance. Patients may find that they have to drink a lot of water to even be able to talk, or they have to stop in the middle of a sentence. You may see their teeth stick to their lips or vice versa.
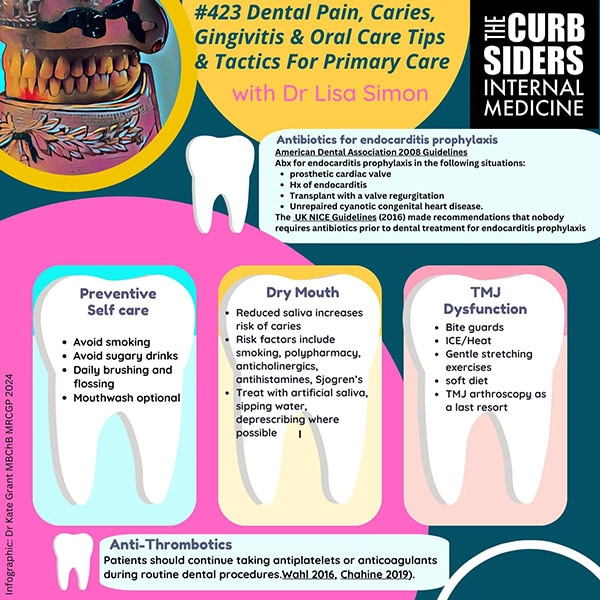
If you can't blame dry mouth on an autoimmune disease, then medications are a common culprit, particularly those that have some anticholinergic side effects, such as antihistamines. Dr Simon gave us some tips for how to manage dry mouth, which include things like sipping on water, artificial saliva, and sucking on sugar-free candy. Please make sure it is sugar free to preserve the teeth while you're taking care of the dry mouth.
Watto: One concern that I hadn't really thought much about, but dentists are much more aware of, is that nifedipine specifically, among some other medications, can cause gingival hyperplasia, especially in patients with poor oral hygiene to begin with. With nifedipine, it seems to be dose- and duration dependent. I tend to use amlodipine for blood pressure rather than nifedipine, just by habit.
Williams: I was aware of it, but unless a patient brings it to my attention, I'm not actively looking for it. It can really bother patients. It's typically painless, but it can be so substantial that it requires surgical intervention to shave down the gums if we are unable to correct it through dose reduction and oral hygiene.
Watto: Dr Simon mentioned that gingival hyperplasia is a bulbous growth of the gum tissue around the teeth. It will regress if you take them off the drug that's causing it, or sometimes by just lowering the dose.
Another thing that commonly comes up in primary care is bisphosphonates. I always worry about these. Am I going to cause osteonecrosis of the jaw in one of my patients? Do they need a drug holiday before having a dental procedure? So if the patient is already on a bisphosphonate and needs dental work, how do we counsel these patients?
Williams: Dr Simon, I believe, is kind of agnostic about the prospect of a holiday from bisphosphonate therapy if the patient is already taking it. We've all gotten the forms that ask whether it can be stopped. But in general, it doesn't seem that there is a whole lot of evidence to support doing that. It's Dr Simon's expert opinion that it isn't necessary to do a drug holiday for patients on bisphosphonates who are scheduled for an extraction or other procedure.
Watto: I've read other sources saying the same thing. Some dentists want them off of bisphosphonates for 2 months beforehand and then resume it after the dental work has healed. But that's not evidence based, according to what we know right now. The incidence of osteonecrosis of the jaw is much higher among patients getting these agents as part of cancer treatment. The risk is much lower in patients with osteoporosis, because the bisphosphonates are oral, which is less intense.
Something that always comes up in practice is the patient on an anticoagulant or antiplatelet agent who is going to the dentist. What do we do with that, Paul?
Willilams: Dr Simon says (and this is consistent with many guidelines) that in general, there's no reason to discontinue the therapy. The dentist can do many things to achieve hemostasis. For example, rather than extracting all of the bottom teeth, you can do them one at a time; or you may need to throw in a suture where you ordinarily wouldn't. Or you might have the patient bite down on the gauze a little harder. But in general, the risk for thrombotic events or stent thrombosis, or something equally scary, is sufficient that they should probably just maintain those therapies. In most instances, dentists don't support stopping the drug because they can do other things to stop the bleeding.
Watto: Dr Simon said she may check an INR level 48-72 hours prior to a dental procedure. It's not 100% necessary, but if a patient's INR is elevated, she might alter the plan.
Click here for the full podcast with Dr Simon.
Credits:
Image 1: The Curbsiders
© 2024 WebMD, LLC
Cite this: Matthew F. Watto, Paul N. Williams. Drugs and Teeth: Prescription Meds With Dental Effects - Medscape - Apr 23, 2024.











Comments