Abstracts
Purpose
We aimed to systematically review the existing evidence and determine the efficacy of MyoRing as a novel method for treatment of keratoconus using meta-analysis.
Methods
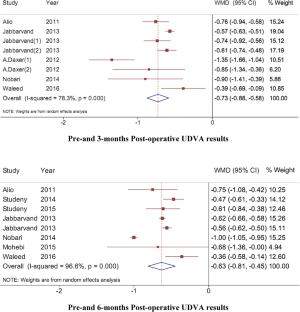
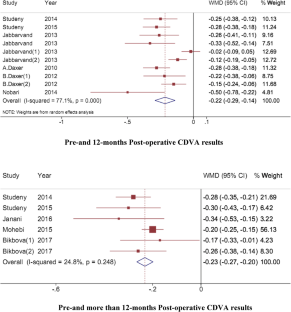
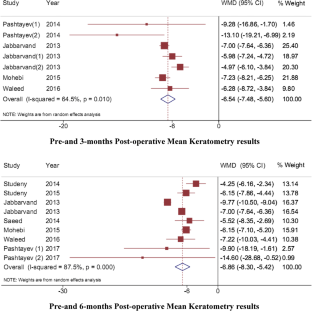
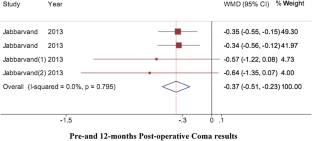
Online electronic search of Medline, ISI Web of Science, Embase, Scopus, and Cochrane Library databases was performed with reference lists of relevant articles for pre–post trials published through August 2017. Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), sphere, cylinder, spherical equivalent (SE), maximum, minimum, and mean keratometry were considered as the visual acuity outcomes. Weighted mean difference (WMD) with 95% confidence interval was used as pooled estimation of intervention efficacy using random-effects meta-analysis. Heterogeneity was measured with the Cochran Q statistic and quantified with the I2 statistic using Stata software.
Results
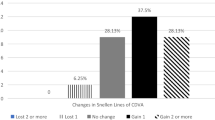
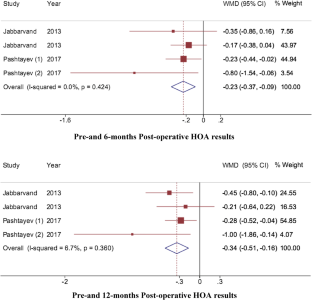
Of the 47 potentially related studies, 21 eligible studies were included in the meta-analysis. The mean of uncorrected distance visual acuity (UDVA) based on LogMAR in patients with keratoconus had a significant change 3 months after implantation/embedding of the complete ring (WMD = − 0.73 (CI = − 0.88 to − 0.58), I2 = 79.9%, p < 0.001). Results support a statistically significance improvement in CDVA, SE, sphere, cylinder, and maximum keratometry after surgical intervention. Range of reported safety index, stability, and efficacy index by included studies was 1.7–2.7, 74–100%, and 0.9–1.96, respectively.
Conclusions
MyoRing is an appropriate treatment option for keratoconus. Findings of this meta-analysis demonstrated that main visual outcomes have been improved 3, 6, and 12 months after the implantation of the complete ring (MyoRing).

Similar content being viewed by others
References
Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, Gordon MO (1998) Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci 39(13):2537–2546
Caporossi A, Baiocchi S, Mazzotta C, Traversi C, Caporossi T (2006) Parasurgical therapy for keratoconus by riboflavin-ultraviolet type A rays induced cross-linking of corneal collagen; preliminary refractive results in an Italian study. J Cataract Refract Surg 32:837–845
Sykakis E, Karim R, Evans JR, Bunce C, Amissah-Arthur KN, Patwary S et al (2015) Corneal collagen cross-linking for treating keratoconus. Cochrane Libr 24(3):CD010621
Kennedy RH, Bourne WM, Dyer JA (1986) A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol 101(3):267–273
Millodot M, Shneor E, Albou S, Atlani E, Gordon-Shaag A (2011) Prevalence and associated factors of keratoconus in Jerusalem: a cross-sectional study. Ophthalmic Epidemiol 18(2):91–97
Gokhale NS (2013) Epidemiology of keratoconus. Indian J Ophthalmol 61(8):382
Davis LJ, Schechtman KB, Wilson BS, Rosenstiel CE, Riley CH, Libassi DP et al (2006) Longitudinal changes in visual acuity in keratoconus. Invest Ophthalmol Vis Sci 47(2):489–500
Zadnik K, Lindsley K (2014) Intrastromal corneal ring segments for treating keratoconus (Protocol). Cochrane Libr 6:011150
Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH (2000) Does ethnic origin influence the incidence or severity of keratoconus? Eye 14(4):625–628
Legare ME et al (2013) Intacs with or without same-day corneal collagen cross-linking to treat corneal ectasia. Can J Ophthalmol 48(3):173–178
Saleem MIHA (2015) Combined cross-linking with femtosecond laser myoring implantation versus combined cross-linking with femtosecond laser keraring implantation in the treatment of keratoconus. J Egypt Ophthalmol Soc 108(3):140
Wollensak G (2006) Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol 17(4):356–360
Kanellopoulos AJ (2009) Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of Keratoconus. J Refract Surg 25(9):S812–S818
Shimmura S, Tsubota K (2006) Deep anterior lamellar keratoplasty. Curr Opin Ophthalmol 17(4):349–355
Al-Tuwairqi W (2015) Comparison of 2 types of intrastromal corneal rings in visual function improvement and Keratoconus outcomes. In: ASCRS. ASOA Symposium and Congress
Saleem MI (2015) Comparison of implantation of 2 ICRS using femtosecond laser for treatment of Keratoconus. In: ASCRS. ASOA Symposium and Congress
Jabbarvand M, Hashemian M, Hashemian H, Bazvand F, Khodaparast M (2014) Femtosecond laser-assisted MyoRing implantation in postoperative LASIK ectasia. J Refract Surg 30(7):462–466
Jabbarvand M, Hashemi H, Mohammadpour M, Khojasteh H, Khodaparast M, Hashemian H (2014) Implantation of a complete intrastromal corneal ring at 2 different stromal depths in keratoconus. Cornea 33(2):141–144
Yildirim A, Cakir H, Kara N, Uslu H (2014) Long-term outcomes of intrastromal corneal ring segment implantation for post-LASIK ectasia. Contact Lens Anterior Eye 37(6):469–472
Hosny M (2014) Complete Ring Versus ICRS Femtosecond Laser-Assisted Implantation for Keratoconus. In: The annual ASCRS and ASOA symposium and congress
Jabbarvand M, SalamatRad A, Hashemian H, Mazloumi M, Khodaparast M (2013) Continuous intracorneal ring implantation for keratoconus using a femtosecond laser. J Cataract Refract Surg 39(7):1081–1087
Raaijmakers LCH, Pouwels S, Thomassen SEM, Nienhuijs SW (2017) Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr 71:441–449
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634
Alio JL, Pinero DP, Daxer A (2011) Clinical outcomes after complete ring implantation in Corneal Ectasia using the femtosecond technology a pilot study. Ophthalmology 118(7):1282–1290
Studeny P, Krizova D, Stranak Z (2014) Clinical outcomes after complete intracorneal ring implantation and corneal collagen cross-linking in an intrastromal pocket in one session for Keratoconus. J Ophthalmol 2014:568128
Studený P, Křížová D, Straňák Z, Kuchynka P (2015) Clinical results after continuous corneal ring (MyoRing) implantation in Keratoconus patients. Ceska a slovenska oftalmologie: casopis Ceske oftalmologicke spolecnosti a Slovenske oftalmologicke spolecnosti 71(2):87–91
Pashtayev NP, Sinitsyn MV, Pozdeyeva NA (2014) Comparative analysis of clinical and functional results of the intrastromal segments and MyoRing implantations in keratoconus using the femtosecond technology. Oftal’mokhirurgiya 1(3):35
Jabbarvand M, Salamatrad A, Hashemian H, Khodaparast M (2013) Continuous corneal intrastromal ring implantation for treatment of Keratoconus in an Iranian population. Am J Ophthalmol 155(5):837–842
Saeed A (2014) Corneal intrastromal MyoRing implantation in keratoconus treatment. J Egypt Ophthalmol Soc 107(2):106
Hosny M, El-Mayah E, Sidky MK, Anis M (2015) Femtosecond laser-assisted implantation of complete versus incomplete rings for keratoconus treatment. Clin Ophthalmol 9:121–127
Daxer A, Mahmoud H, Venkateswaran RS (2010) Intracorneal continuous ring implantation for keratoconus: one-year follow-up. J Cataract Refract Surg 36(8):1296–1302
Bikbov M, Bikbova G (2012) Intrastromal corneal MyoRings with corneal collagen cross-linking in keratoconus treatment. Ophthalmosurgery 4:6–9
Zhadan VA, Lebedev OI, Kalyzhnikova EA (2014) Intrastromal keratoplasty with MyoRing implantation in surgical treatment of keratoconus. Preliminary results. Oftal’mokhirurgiya 1(3):31
Daxer A, Ettl A, Hörantner R (2016) Long-term results of MyoRing treatment of keratoconus. J Optom 10(2):123–129
Daxer A (2012) MyoRing for central and noncentral keratoconus. Int J Keratoconus Ectatic Corneal Dis 1:117–119. Accessed Mar 2019
Janani L, Jadidi K, Mosavi S, Nejat F, Naderi M, Nourijelyani K (2016) MyoRing implantation in keratoconic patients: 3 years follow-up data. J Ophthalmic Vis Res 11(1):26–31
Daxer B, Mahmood H, Daxer A (2012) MyoRing treatment for keratoconus: DIOPTEX PocketMaker vs Ziemer LDV for corneal pocket creation. Int J Keratoconus Ectatic Corneal Dis 1:151–152
Nobari SM, Villena C, Jadidi K (2014) Predictability, stability and safety of MyoRing implantation in Keratoconic eyes during one year follow-up. Iran J Ophthalmol 26(3):136–143
Mohebbi M, Hashemi H, Asgari S, Bigdeli S, Zamani KA (2016) Visual outcomes after femtosecond-assisted intracorneal MyoRing implantation: 18 months of follow-up. Graefes Arch Clin Exp Ophthalmol 254(5):917–922
Al-Tuwairqi WS, Osuagwu UL, Razzouk H, AlHarbi A, Ogbuehi KC (2017) Clinical evaluation of two types of intracorneal ring segments (ICRS) for keratoconus. Int Ophthalmol 37:1185–1198
Bikbova G, Kazakbaeva G, Usubov E (2018) Complete corneal ring (MyoRing) implantation versus MyoRing implantation combined with corneal collagen crosslinking for keratoconus: 3-year follow-up. Int Ophthalmol 38(3):1285–1293
Pashtaev NP, Pozdeeva NA, Sinitsyn MV (2017) Comparative analysis of corneal aberrations after intrastromal segments and MyoRing implantation using femtosecond laser in patients with keratoconus. Vestn Oftalmol 133(3):3–8
Mahmood H, Venkateswaran RS, Daxer A (2011) Implantation of a complete corneal ring in an intrastromal pocket for keratoconus. J Refract Surg 27:63–68
Daxer A (2010) Adjustable intracorneal ring in a lamellar pocket for keratoconus. J Refract Surg 26(3):217–221
Mojaled Nobari S, Villena C, Jadidi K (2015) FullRing Intracorneal Implantation in Corneas with Pellucid Marginal Degeneration. Iran Red Crescent Med J 17(12):e28974
Daxer A (2014) Corneal thickness after MyoRing implantation for keratoconus. Int J Keratoconus Ectatic Corneal Dis 3(1):15
Keratoconus International. https://www.keratoconusinternational.com/cisis-myoring/myoring-long-term-results
Piñero DP, Alio JL (2010) Intracorneal ring segments in ectatic corneal disease—a review. Clinical Exp Ophthalmol 38(2):154–167
Mastropasqua L, Nubile M, Salqari N, Mastropasqua R (2018) Femtosecond laser-assisted stromal lenticule addition Keratoplasty for the treatment of advanced keratoconus: a preliminary study. J Refract Surg 134(1):36–44
Sammour HM, Ismail MM, Abdelghany AI, Shafeek MA (2017) Comparative study between Myoring and Ferrara Ring Intracorneal implantation using femtosecond laser for treatment of Keratoconus. Egypt J Hos Med 68:910–922
Acknowledgements
We thank native English speaking editor from Birmingham Research Park (United Kingdom) for improving the use of English in the manuscript.
Funding
This study was partially supported by funds from Vice-Chancellor for Research of Iran University of Medical Sciences (IUMS), Tehran, Iran (Grant Number:94-05-27-27457). The funding sources had no role in study design, data collection, analysis, interpretation, and preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
LJ, KJ, and FN conceived the idea and designed the study. KT, LJ, and FN collected data, reviewed literature, and extracted data. KT, LJ, and MS, and MD participated in the analysis of data and interpreted the results. LJ, MD, and MS conceived the study aims and design, provide the data and measures, and designed the analysis. KJ, FN, and SJH reanalyzed data, made substantial contribution to interpretation of data, drafting the manuscript and revising it critically for important intellectual content and final approval of the version to be submitted and any revised version. All authors reviewed, discussed, provided critical comments, and approved the final manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Janani, L., Tanha, K., Najafi, F. et al. Efficacy of complete rings (MyoRing) in treatment of Keratoconus: a systematic review and meta-analysis. Int Ophthalmol 39, 2929–2946 (2019). https://doi.org/10.1007/s10792-019-01121-9
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1007/s10792-019-01121-9